| |
| |
 |
| |
 |
| |
|
| |
Abnormal collection of small or large blood vessels produces red birthmarks. Their pink, red, crimson or blue color depends on the size of the blood vessels and whether they are predominantly capillaries, arterioles or veinules. Oxy hemoglobin in arterial blood and de-oxy hemoglobin in venous blood, both absorb lasers of certain wavelengths & get heated. This heat is transmitted to the vessel wall which seals them off and the birthmark starts fading gradually.
Pulsed dye lasers with 595 nm, IPL with 590 cut off filter & 1064 nm short pulse Nd:YAG lasers are most effective in treating vascular birthmarks. Multiple treatment sessions at periodic interval are necessary and their number depends on the type of the lesion. |
| |
|
| |
HEMANGIOMAS |
| |
The name hemangioma is derived from three words: ‘haem‘ means blood, ‘angios‘ means blood vessel and ‘oma ‘ means tumor. Hemangiomas are birthmarks that are found in approximately 10% of babies by the time of their first birthday, making it one of the most common types of birthmarks. Many hemangiomas are not present at birth, but appear within the first few weeks or months of the child‘s life. Medical science as of today does not know exactly what causes hemangiomas, though they do rarely run in families. In addition, a parent who has one child with a hemangioma does not have an increased likelihood of having another child with one. Hemangiomas are found three times more commonly in girls than in boys and are also more common in premature infants. |
| |
|
| |
Types of Hemangiomas |
| |
There are three main varieties of hemangiomas: superficial ‘strawberry‘, deep ‘cavernous‘, and combined. The strawberry hemangioma is located on the skin and is bright red and contains a well defined border. The deep or cavernous hemangioma starts from beneath the skin and is characterized by soft mass that is bluish or skin colored. As the name implies, the combined hemangioma has both components, superficial like the strawberry and deep like cavernous hemangioma.
Hemangiomas also can be categorized according to their distribution as:
Since the localized spread does not involve structural deformities, hence it occurs with lesser complications. In the segmental and diffuse forms, there are greater complications.
|
| |
|
| |
Natural Course of Hemangioma
|
| |
|
| |
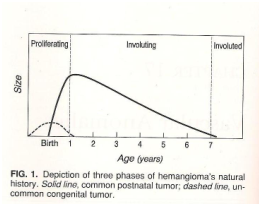
All hemangiomas if not treated or interfered with, pass through following four phases:
- Proliferating: Stage of vigorous growth
Most often, hemangiomas are not present or noticeable at birth. Within first one to two months, however, the red marks become visible (Initial macular blemish). From first month to the age of six to twelve months, they generally grow rapidly. (Proliferating phase). After this period, their growth slows down and around twelve to eighteen months they begin to shrink or ‘involute‘. Thirty percent of hemangiomas disappear on their own by the time the child is three years old and 50% are gone by the 5th birthday. By the time child reaches the age of nine years, 80-90% are gone. In all, approximately half resolve completely without any form of treatment and without leaving residual marks. (Fig. 1)
Uncommon forms are rapidly involuting hemangiomas (RICH) or noninvoluting hemangiomas (NICH)
|
| |
|
| |
Why Treat The Hemangioma?
|
| |
|
| |
In some cases, however, treatment is recommended. Some can cause medical problems, such as bleeding, ulceration, crusting or infection. In addition, some hemangiomas are in areas that can affect a vital organ, such as an ear (Fig. 2), an eye (Fig. 3), or a windpipe. Some also grow very rapidly and can cause deformation and / or destruction of the surrounding tissues (Fig. 4). In addition, the location of a hemangioma can be emotionally traumatic for the parents, making removal with cosmetic laser surgery an option for parents to consider seriously. This is particularly true if the hemangioma is in an area that can become easily irritated or ulcerated, such as in scalp, skin folds or in areas where clothing commonly rubs. In addition, having a hemangioma in an exposed area, such as on the face, neck or arms can cause social embarrassment to a child, particularly when the child begins interacting with peers.
|
| |
|
| |
Treating Hemangiomas with Cosmetic Laser Surgery
|
| |
|
| |
To remove strawberry hemangiomas, a pulsed dye laser or IPL can be an effective treatment. Generally, a series of treatments spaced four to six weeks apart are needed. For deep or cavernous hemangiomas because they are characterized by raised tissue, a deep reaching 1064 nm Short Pulsed Nd:YAG laser is needed.
|
| |
|
| |
‘Masterly Inactivity‘ Vs ‘Timely Intervention‘
|
| |
|
| |
Because of the high rate of spontaneous resolution and non availability of an effectively curative treatment in the past, ‘ Masterly Inactivity‘ was advocated and practiced by physicians all over the world. But as much as 50% of those which spontaneously resolve leave behind a crumpled skin called ‘anetoderma‘ (Fig.5) as well as some objectionable marks. (Fig.6)
Since the advent of lasers during last decade, the scenario has changed completely. A properly selected laser for the type of hemangioma effectively closes the blood vessels non-invasively and permanently, without leaving behind any scar or marks on the skin. Therefore, ‘Timely Intervention‘ with the cosmetic laser surgery may be the right choice for you and your child. Evidence suggests that hemangiomas are best treated early in life prior to their rapid expansion phase. Therefore now ‘Timely Intervention‘ really means ‘Earliest Intervention‘ with Laser. (Fig. 7 A & B) Even the long term results are excellent with minimal or no scars left behind. (Fig. 8 A & B)
Below is an overview of the stage-wise potential for laser treatments
|
| |
|
| |
Initial Macular Blemish
|
| |
|
| |
Early macular lesions are usually small in size and therefore can be treated without subjecting the child to general anesthesia. Successive sessions at 3 week interval have proved most effective.
|
| |
|
| |
Stage of Vigorous Growth
|
| |
|
| |
This stage generally occurs between 3 and 9 months of age and is often accompanied with bleeding , ulceration and infection. Both Pulsed Dye Laser (PDL) & 1064 nm short pulse Nd:YAG have proved their best for the treatment of hemangioma in this stage. As the hemangiomas are growing very rapidly, first few treatments may be utilized just to halt their progress and therefore, one may not notice any visible improvement in the lesion size or color.
|
| |
|
| |
Involution and Involuted stage
|
| |
|
| |
The procedure involved in the involution of hemangiomas is still not very clear. The various types of lasers that have proved effective in this stage are:
- PDL treatment: After the involution, the leftover telangiectasia is best corrected with pulsed dye laser, with the standard settings for a cosmetic clearance. However, since lasers have limited penetration, they fail to work in case of deep hemangiomas. Moreover, it has side effects such as ulceration, combined with scarring and hypopigmentation.
- The Pulsed 1064 nm Nd:YAG laser: This has been the latest development in the treatment of haemangiomas. These are often used to correct exophytic, ulcerated and subcutaneous haemangiomas. It has proved successful in checking the growth of hemangiomas in 70% of patients.
Localized lesions can be subjected to laser without anesthesia, but larger, complicated spreads (like segmental and diffuse forms) and those around the eyes should be done with short general anesthesia.
|
| |
|
| |
Other Treatment Modalities
|
| |
|
| |
Combination treatment of laser (PDL / IPL) and corticosteroids are also often used. Surgical intervention has also been a choice especially in cases with excess fibro fatty tissue deposits and superfluous skin left behind after involution. Surgical intervention should be done at an early stage, when the features of the child and body appearance are at a formative phase. Carbon dioxide laser are used in the cosmetic correction of the surgical scar and PDL used for the removal of telangiectasia deposits.
LakshyaKiran Cosmetic Laser Center has twelve years experience in laser treatment of red birthmarks and is a recognized expert in the treatment of the entire spectrum of congenital vascular skin conditions having Indian record of largest number of hemangiomas treated with laser to its credit.
|
| |
|
| |
PORT-WINE STAINS (PWS)
|
| |
|
| |
Port wine stains can occur anywhere on the body and may rarely be associated with underlying abnormalities of the eye and brain. Port wine stains show diffuse collections of dilated capillaries in the dermis. Newer treatment modalities using pulsed dye laser 595 nm (yellow), and IPL with 590 cut off filter can improve or eliminate many of these lesions.
Treatment of PWS
Fortunately new advances in laser surgery have enabled us to remove or improve many of these conditions. PWS birthmarks respond remarkably well to laser treatment. When the laser is used to treat port-wine stains, no cuts or punctures are made. The laser energy penetrates through the skin to shrink the abnormal blood vessels that are the cause of these birth marks. Port-wine stain birthmarks respond remarkably well to laser treatment. The abnormal blood vessels that cause these marks are reduced in size by the laser. This results in a lightening of the treated area. Usually it takes more than one laser treatment. The facial plastic surgeon often uses the minimum laser intensity possible. The low intensity requires many treatments. However, the low intensity also preserves as much of the healthy tissue as possible. This produces an aesthetically pleasing result. (Fig. 9) Most of these laser surgeries are performed on an outpatient basis in an office set up.
|
| |
|
| |
VENOUS MALFORMATION
|
| |
|
| |
Venous Malformations (VM) are present at birth, but are not always evident. These slow flow anomalies manifest either as a faint blue patch or a soft blue vascular mass. They can be either localized or extensive within an anatomic region, minor or distorting and typically located on face, limbs or trunk. They can be hereditary, occur in internal organs and are usually solitary. Often they are incorrectly labeled as ‘cavernous hemangioma ‘.
VMs are easily compressible and exhibit increased swelling when dependent. They grow proportionate with the child, expand slowly and often enlarge during puberty. An extremity VM rarely produces limb length discrepancy, sometimes causes structural weakening of the bony shaft and pathologic fracture. MRI is the most informative imaging modality.
Treatment of a VM is indicated for appearance or for functional problems. Internal lesions require image guided sclerotherapy or blockage. Cutaneous, subcutaneous and some of the superficial muscular lesions can be successfully managed with 1064nm Short Pulsed Nd:YAG laser energy delivered per cutaneously in multiple sessions (Fig. 10 A & B). It avoids surgery, resultant scar and possible damage to important surrounding structures as lasers have the unique property to get absorbed and exhibit effect only on the target.
|
| |
|
|
|
 |